“In this world nothing can be said to be certain, except death and taxes” said Benjamin Franklin. While some might brag about how they can avoid the latter, no-one has or will escape the former. What we do avoid, however, is talking about it.
In February of 2015 the Supreme Court of Canada struck down the existing laws covering assisted suicide, calling for new legislation that would allow mentally competent patients to end their lives with the help of someone else, most likely a physician, while protecting others against coercion. While the federal government has tried to put the issue on the back burner, others have weighed in on all sides of the argument, citing statistics from other jurisdictions which already have such a law on the books.
In June of 2014, after extensive consultation and a change of government, the Quebec government passed Bill 52, An Act Respecting End-of-Life Care, and published guidelines in a report entitled “Dying With Dignity” which lays out how this is to be managed and conditions that must be met, and recognizes the primacy of the patient’s wishes. The law will come into force on January 1, 2016 but Quebecer’s can begin asking for the procedure starting December 10, 2015.
While the arguments on all sides have concentrated on assisted suicide, almost lost in the discussion is a problem confronting people who know their life-span will be limited because of the nature of their ailment, but have no immediate wish to end their lives. Their concern is finding a way to live as comfortably as they can, for as long as they can, while letting nature take its inevitable course, without unnecessary intervention, and in surroundings that feel as much like home as possible.
We are urged to keep our Power of Attorney for Property (or whatever the appropriate terminology in different provinces) up to date, but the POA for Personal Care is less likely to be cause for discussion among family members. “The parents are okay….we’ll talk about it another time.” But, do we really know what Mum wants if she is in an accident, or not in a position to make medical decisions? Does she want “heroic measures” taken no matter what her condition? Does she want to spend her last days at home, and if so, how will you manage it?
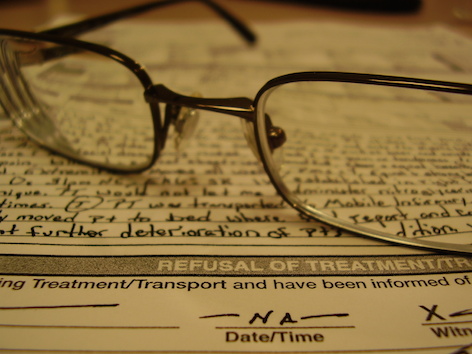
The best way to ascertain her wishes is to include an Advance Directive within the POA for Personal Care. If you give someone Power of Attorney for Property, that person can act for you at any time. However, a Power of Attorney for Personal Care only kicks in when you are unable to make medical decisions for yourself. As usual, there are different types of advance directives in Canada, with each province using slightly different language, and with different laws for these documents.
The Canadian Elder Law website has links to a variety, but not all jurisdictions across Canada. The best advice is to consult a lawyer who is an expert in this field.
In 2012, Senator Elizabeth Hubley spoke in the Senate about an all-party committee report and said that palliative care now has much more recognition that in the past and that about 90 per cent of all deaths can benefit from palliative care. However, only 16 to 30 percent of those people actually receive it. The majority of people who need it still cannot access it.
This creates a serious challenge for the caregiver. Assuming you know what your spouse or your parent wants when it becomes clear that they are approaching the end of life, how do you find the best care? Can you provide it yourself? Do you need help? If you do, how can you find it? There are a variety of organizations across Canada, prominent among them the Canadian Hospice Palliative Care Association. Their website provides links to all provinces.
However, although they offer information on accessing at-home help – limited though that may be in some areas – there is a serious lack of stand-alone hospices or those associated with other health care hubs where those reaching the end of life can live comfortably with their family and friends by their side in a home-like environment.
A CARP member relates how she was able to have her late husband spend his last weeks in relative comfort at home. While he was in hospital at Sunnybrook Hospital in Toronto, they were approached by a team from the Temmy Latner Centre for Palliative Care.
“When the young doctor asked if we knew what “palliative care” was, my husband and I looked at each other, neither wishing to put into words the situation we were facing. While we hesitated to reply, she assured us that their aim was to help provide everything he needed – including regular visits from doctors, nurses or therapists to keep him comfortable and close to pain-free as possible. Through the local Community Care Access Centre we would have use of the equipment we needed, including a hospital bed. If his doctor – who made regular visits – wasn’t available in any kind of emergency, I had another number to call. Within minutes the doctor on call would phone back.”
“The care was superb, and I couldn’t have done it without them. But now that I’m completely on my own, with no close family near me, I wonder what will happen if I’m in a situation where I become terminally ill? Is there a hospice where I could go?”
The short answer is that these facilities are few and far between, an important subject which we will continue to explore in coming issues of CARPActionOnLine.
